Written by Pendell Meyers, with edits by Steve Smith
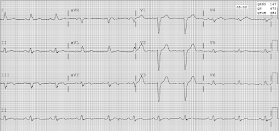
A male in his 80s old had acute onset of chest pain. Here is his first ECG, time zero:
Sinus rhythm with left bundle branch block. There is concordant STE in leads II, V5, and V6. It may not reach a full millimeter, but the QRS is so small that we should make an exception here. It is proportionally large concordant ST elevation!
The cath lab should be activated, but apparently it was not. Instead, another ECG was recorded at time 46 minutes:
The cath lab was activated and a circumflex occlusion was opened and stented, with a door to balloon time of 3 hours.
Here are ECGs recorded after reperfusion:
As an explorative substudy of our validation of the modified Sgarbossa criteria, we studied T-wave inversion. We looked at serial ECGs on patients with acute coronary occlusion ACO) who underwent reperfusion and compared to serial ECG on patients without ACO. Unfortunately, as a result of our multisite study in which ACO came from many institutions and controls from one institution, only 6 of 45 patients with ACO and reperfusion had serial ECGs available, and all 245 patients without ACO had serial ECGs available.
See this post: Classic Evolution of Wellens' T-waves over 26 hours
See these posts for Pseudonormalization of Wellens' waves (re-occlusion):
This one is EXTREMELY subtle:
A male in his 80s old had acute onset of chest pain. Here is his first ECG, time zero:
 |
| What do you think? |
Sinus rhythm with left bundle branch block. There is concordant STE in leads II, V5, and V6. It may not reach a full millimeter, but the QRS is so small that we should make an exception here. It is proportionally large concordant ST elevation!
The cath lab should be activated, but apparently it was not. Instead, another ECG was recorded at time 46 minutes:
The cath lab was activated and a circumflex occlusion was opened and stented, with a door to balloon time of 3 hours.
Here are ECGs recorded after reperfusion:
 |
| ST deviation has resolved. There is already terminal T-wave inversion in leads III and aVF. |
 |
| T-waves are inverting in the affected leads. This is analogous "Wellens' waves" of the inferior and lateral leads, in the presence of LBBB! |
As an explorative substudy of our validation of the modified Sgarbossa criteria, we studied T-wave inversion. We looked at serial ECGs on patients with acute coronary occlusion ACO) who underwent reperfusion and compared to serial ECG on patients without ACO. Unfortunately, as a result of our multisite study in which ACO came from many institutions and controls from one institution, only 6 of 45 patients with ACO and reperfusion had serial ECGs available, and all 245 patients without ACO had serial ECGs available.
When this pattern was retrospectively defined as being either 1) present in at least two
contiguous anterior or inferior leads in at least two consecutive ECGs prior to reversal or 2) deeper than 3 mm in two contiguous leads (requiring only one ECG), it was found to be predictive of reperfused ACO (either spontaneously prior to catheterization or with mechanical reperfusion) with derived sensitivity and specificity of 5 of 6 [83% (95% CI 36–99%)] and 241 of 245 [98% (95% CI 96–99%)]. This is preliminary low-level evidence which suggests that terminal T-wave inversion as a sign of reperfusion is sometimes still applicable in the setting of abnormal QRS such as LBBB and likely ventricular paced rhythm as well.
Meyers HP. Jaffa E. Smith SW. Drake W. Limkakeng AT. Evaluation of T-Wave Morphology in Patients With Left Bundle Branch Block and Suspected Acute Coronary Syndrome. Journal of Emergency Medicine 51(3):229-237; September 2016.
We (Meyers and Smith) also published a case of Wellens' syndrome (involving the LAD) in LBBB:
As a very brief review for new readers, terminal T-wave inversion is an expected finding with reperfusion of acute coronary occlusion which is well established in the presence of normal QRS conduction (no LBBB, paced rhythm, etc). It was first described by Wellens and colleagues in the anterior leads in the setting of an acute proximal LAD stenosis, and later it was more fully understood as a transient phase of reperfusion soon after acute coronary occlusion. When it was first described, it was initially divided into "pattern A" and "pattern B", characterized by biphasic terminal T-wave inversions then full, symmetric T-wave inversions, respectively. In reality these are not separate presentations of the disease but simply two different time periods during the progression (see progression below).
Furthermore, though Wellens described this pattern only in LAD leads, it is clear that it occurs in inferior and lateral leads as well.
See this case of inferolateral Wellens' syndrome, with subsequent re-occlusion and pseudonormalization of T-waves.
Dynamic T-wave inversions in the setting of left bundle branch block
As a very brief review for new readers, terminal T-wave inversion is an expected finding with reperfusion of acute coronary occlusion which is well established in the presence of normal QRS conduction (no LBBB, paced rhythm, etc). It was first described by Wellens and colleagues in the anterior leads in the setting of an acute proximal LAD stenosis, and later it was more fully understood as a transient phase of reperfusion soon after acute coronary occlusion. When it was first described, it was initially divided into "pattern A" and "pattern B", characterized by biphasic terminal T-wave inversions then full, symmetric T-wave inversions, respectively. In reality these are not separate presentations of the disease but simply two different time periods during the progression (see progression below).
Furthermore, though Wellens described this pattern only in LAD leads, it is clear that it occurs in inferior and lateral leads as well.
See this case of inferolateral Wellens' syndrome, with subsequent re-occlusion and pseudonormalization of T-waves.
See this post: Classic Evolution of Wellens' T-waves over 26 hours
See these posts for Pseudonormalization of Wellens' waves (re-occlusion):
This one is EXTREMELY subtle:
A Middle-Age Male with Chest Pain that Recurs in the ED
Pseudonormalization of Wellens' Waves
Subtle LAD Occlusion with Pseudonormalization of Wellens' Waves.
This one shows why patients with Wellens' syndrome who do not go immediately to the cath lab need continuous 12-lead ST Segment monitoring:



final diagram (Occlusion-Reperfusion) is exceptional !
ReplyDeletemerci - Al
That's Pendell's doing!
DeleteThanks for the final break down on Wellens syndrome. As a Paramedic stumbling through any random articles I can scrounge it seems like most describe Wellens as anterior only with the type 1 and type 2. A lot of articles put a footnote in stating that the pattern may present elsewhere but this description is certainly not emphasized in the main body. I think the Facebook memes are especially guilty of this when showing pics of different types of syndromes. I also thought it was very interesting to hear it’s progression of changes. Wish that was better published. Thanks
ReplyDeleteIt is mostly published here on this blog.
DeleteWhen I teach about wellens and reperfusion to my residency group, I like to offer this analogy to make it more entertaining and memorable: Imagine you were a martian who just discovered that humans exist on earth. You look through your telescope and see a middle aged man walking down the street with a small child beside him. You might conclude that there are two distinct types of humans - type A which are taller and smarter, and type B which are small and clumsy. In reality they are just two different time periods in the same general progression, which you don't understand when you see snapshots of them for the first time but you come to learn as you watch them progress in individual cases and see the patterns play out.
DeleteSo many great cases on this blog of this phenomenon.
Nice case. I’ll offer an alternative approach for how to quickly recognize that the 1st ECG in this case of a patient with new-onset chest pain represents acute coronary occlusion until proven otherwise. It is based on 2 premises. The 1st, is that the direction of the ST-T wave in the 3 key leads for diagnosing RBBB or LBBB ( = leads I, V1, V6) should be oppositely directed to the direction of the last QRS deflection in these 3 leads. This relationship IS preserved as it should be in lead V1 — since the last QRS deflection in V1 is the deep negative S wave (therefore the T in V1 is appropriately positive). The relationship is equivocal in lead I. But, there is NO doubt that the upright ST-T wave in lead V6 should not be. The 2nd premise in my system relates to the concept of looking for ST segment elevation (or hyperacute ST segments) in leads that should not show this. The shape of the T waves in leads II, V5, and V6 is clearly abnormal (and looks hyperacute) in this 1st ECG, in view of the minimal QRS amplitude in these leads. In a “high prevalence” population (ie, the patient in this case is 80yo, and he is having new-onset chest pain) — this 1st ECG should unequivocally be indication for immediate cath. These ECG abnormalities become all the more striking in the 2nd ECG — which now, in addition to hyperacute ST-T waves, shows ST elevation in leads that should not show elevated ST segments (ie, in leads II, III, aVF, V4, V5, V6). THANKS to Drs. Pendell Meyers and Steve Smith for continuing to increase awareness of how acute coronary occlusion can be diagnosed in many patients despite the presence of LBBB.
ReplyDeleteThanks Ken! Totally agree that the T-waves are hyperacute in addition to all the other findings, should have written that in the same place as the ST segments discussion.
Deletevery interesting discussion, gentlemen.
ReplyDeletehypervigilance , and awareness seems to be crucial. and when unclear, or less clear, i guess repeat the ekg sooner than later.
thank you, all three.
What is the significance of concordance here and what we are trying to rule out or try to see through these concordance.
ReplyDeleteIn normal LBBB (without ischemia; i.e., without coronary occlusion), the ST segment should never be in the same direction as the majority of the QRS (i.e., should never be "concordant" with the QRS). In the first ECG, it is concordant in II, V5 and V6. If there is 1 mm of concordance in just one lead, that is STEMI.
DeleteSir i want to know about the criteria of hyperacute T wave i am just confused with lots of data please tell about perfect criteria of hyperacute and TALL T wave.
ReplyDeleteWow. that is too much to explain all at once. Just keep reading the blog and you'll get it.
DeleteThanks sir.
Delete@ Anonymous — I agree totally with Dr. Smith that the "best way" to recognize a "hyperacute" ST-T wave is to keep looking at hundreds (thousands) of ECGs — and eventually your mindset will develop the picture to allow near-instant recognition (sometimes without exactly knowing "why" ... ). That said — I'd propose an answer to your question entails an ST-T wave that "looks-more-prominent-than-it-should-be" in the lead you are looking at (ie, in comparison to the amplitude and shape of the QRS in that lead). Sometimes it looks as if the ST segment is "trying" to raise itself up, but "hasn't yet" been able to do so ... And of course it helps when you think you are seeing one lead with potentially "hyperacute changes" if on a second look, you detect subtle-but-real abnormalities in at least several other neighboring leads. And again, once your brain has encountered enough hundreds and hundreds of tracings paying the right amount of attention to your attempts at interpretation — you'll begin to instantly recognize this pattern.
DeleteNovice question....In ECG 1, Is the final deflection in lead 2 positive or negative?
ReplyDeletethe ST-T is all positive. not sure what you mean.
Delete* last QRS deflection positive or negative in lead 2?
DeleteIt is all positive. The end does not go below PQ jct. Anyway, it is the majority of the QRS that matters, and that, in fact, is the area under the curve (I believe)
DeleteIn ECG 1 and 2,in lead V5, is it concordant ST elevation or just a proportionally tall T wave?
ReplyDeletethere is some ST elevation, though minimal
DeleteHi there, firstly thanks for the great ECGs & post as always! :D
ReplyDeleteAs a novice ECG reader I find myself time and time again thrown off by ST-Segments like the ones in V2-V4 in the first ECG especially in LBBB. To me it looks like relevant STE on first glance and I'm a bit confused. Would love if you could explain or point me in the directions of some articles. My books aren't really helpful.
There is indeed ST elevation. But it is not ischemic ST elevation. Many conditions cause ST elevation: normal variant, LVH, LBBB, pericarditis. And ischemia. The trick is to be able to differntiate ischemic ST elevation from ST elevation due to these other conditions. LBBB is one.
DeleteAny of the books that I recomment would help
Delete