This was written by Sam Ghali (), with a few edits by me.
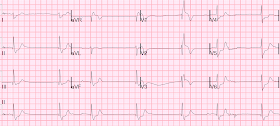
52-year-old lady presents to the Emergency Department with 2 hours of chest pain, palpitations & SOB. She is somewhat hypertensive, but her vital signs are otherwise normal. Here is her 12-Lead ECG:
 |
| There’s a sinus rhythm at around 70 bpm. There are Q-waves in the inferior leads (II, III, AVF) with ST-Elevations. These elevations meet STEMI criteria (≥1mm in 2 contiguous leads). However, old MI w/aneurysm morphology (persistent ST-Elevation) can look just like this. Looking closer, we see clear ST depression in the lateral limb leads, I and AVL. While this may be change that is reciprocal to an Acute/Subacute Inferior STEMI, the problem is that LV aneurysm may also manifest with this reciprocal change. [This is further complicated here by the fact that this patient has LVH & strain pattern (R wave in AVL > 11mm) which can also account for these changes] |
Is this a Acute/Subacute STEMI or an Old MI with persistent STE/ “Aneurysm Morphology”?
What are some clues to help us differentiate between the two in this scenario?
1. Ischemic Hyperacute T waves (Tall, round, symmetric, vs the “pointy” peaked-T’s of HyperK), are often a clue to ischemia. In STEMI, they are generally upright and large in proportion to the QRS. The T-waves here are not upright or particularly large. So this argues against acute STEMI. However, we must also keep in mind that in Subacute STEMI (6 hours duration) Hyperacute T-waves will decrease in amplitude and eventually invert as infarction progresses (indicating less viable myocardium) similar to what we see here.
2. There are Qr-waves in the inferior leads with minimal r-wave amplitude. In acute/subacute STEMI, the natural progression is for the Q-waves to increase in size, while the amplitude of the R-waves diminish. These will ultimately develop into a final mature “Qr-waves”. Therefore, catching these waves in their “transition period” would imply an evolving STEMI. Are the waves seen here still in the process of evolution, or is this their final state? It is difficult to answer this question based on this single ECG alone. A word of caution: while anterior aneurysm almost always has QS-waves or tiny r-waves followed by an S-wave (rS-wave), inferior aneurysm may present with QR-waves (and, of course, Qr-waves)
3. Old MI w/Aneurysm will show moderate ST Elevation, as seen here. We don’t see excessive ST Elevations (“Tombstones”) that would suggest acute STEMI, but clearly acute STEMI can certainly present with moderate ST Elevation as well.
4. Although not always available a prior ECG is probably the most helpful piece of information in these cases. Without them the diagnosis is often tough and one must often rely on other clinical data- serial ECG’s, troponin, on-going chest pain, etc.
5. Most, but not all, ECG “aneurysm morphology” is associated with an actual aneurysm on Echo (see this case with ED bedside echo). So a bedside Echo showing a dyskinetic inferior wall may be helpful in this scenario as well, but this wasn't the case here. Bedside echo did show inferior wall motion abnormality, but this isn't helpful in distinguishing the two entities in the differential at hand.
6. Finally, prolonged duration of MI (subacute MI) can mimic LV aneurysm. This is a case from Dr. Smith's files of a patient with no prior history of MI who presented with 12 hours of chest pain:
 |
There are Qr-waves in inferior leads, and reciprocal ST depression in aVL.
Notice also that no lead has 1 mm of ST elevation.
This turned out to be a subacute inferolateral STEMI.
Immediate angiography showed 100% acute RCA occlusion and 99% circumflex (dual culprit lesions). Maximum troponin I was 197 ng/mL (huge MI) |
Case continued:
So is this patient having a STEMI? Should the cath lab be activated?
This case is tough. I will say that without a previous ECGs, given this patient's active/persistent chest pain and positive troponin, I very likely would have activated the cath lab. In this particular case however, a review of the chart revealed the following ECG from an admission 3 weeks prior:
 |
Comparing the two ECGs, we see that her presenting ECG is largely unchanged.
|
Therefore, the changes in the inferior leads seem to indicate "persistent ST-Elevation", which is typically the result of an unreperfused, full thickness ("transmural") MI. Naturally, in the reperfusion era, this entity has become much more rare than it used to be.
So why did this patient have this persistent ST-Elevation/Aneurysm morphology?
Interestingly, in further review of the chart it seems the patient was admitted to the hospital floor 3 weeks prior for an unrelated surgical procedure. She complained of nausea that night and the following 3 ECGs were obtained over a period of 10 minutes:
Just 2 minutes later:
8 minutes after that:
 |
There is an obvious, large inferior STEMI with marked ST-Elevation in II, III, & AVF, along with significant depression in I & AVL. We can see that there is evolution of the elevations, worsening reciprocal change, as well as evolution of posterior involvement (right precordial R-waves with ST depression)
|
There was very little documentation surrounding these ECGs. It appears that the patient was not experiencing any chest pain, and therefore unfortunately these ECGs were not acted upon. The following morning on rounds the ECGs were noted and the patient eventually underwent cardiac catheterization (>18 hrs after later!) She was found to have 100% occlusion of the mid RCA(culprit lesion), which gave rise to acute marginal, PDA and PL branches(which explains the posterior involvement). She received PCI with 2 drug-eluting stents in overlying fashion. She had a very large troponin leak. Convalescent Echo showed 30-35% LF EF, inferior wall akinesis, and persistent severe posterior wall hypokinesis.
Take a look at the patient’s ECG taken the morning during rounds (still prior to cath):
 |
Compared to the obvious STEMI ECGs from the night before, we can see that the degree of inferior ST elevation has diminished, along with the amplitude of the R-waves. These waves are still in the process of transitioning to their mature and final state as Qr-waves. These features are indicative of evolving infarction and of decreasing myocardial viability. Note also the T-wave evolution, from large, tall hyperacute T-waves to smaller biphasic/inverted T-waves.
Also interestingly, note the increased R-wave amplitude in lead V2. This is a result of posterior wall infarction. The R-wave amplitude in V2 is the sum of the anterior forces from the anterior wall minus the forces of the posterior wall which are directed opposite this lead. Since there are now no opposite forces, the anterior forces predominate even more, resulting in increased R-wave amplitude in V2. What we are seeing is essentially "posterior Q-waves".
|
To better appreciate the electrocardiographic evolution of this MI, take a look at the chronological progression in the inferior leads:
 |
Note the evolution of the R-waves as we catch them in transition to their final/mature QR wave state. Also note the evolution of the T-waves.
|
Back to the patient’s present visit (3 weeks after this initial visit). She was again admitted to the hospital, and there was no further evolution of her ECG. She was maximized on medical therapy, her pain subsided, and her max troponin was only slightly elevated (NSTEMI). After a short stay, she was discharged home.
Learning Points:
1. Acute/Subacute STEMI vs LV Aneurysm can be tough to differentiate. Inferiorly, the distinction can be much tougher than anteriorly. (This is due to the fact that inferiorly we see the development of QR waves as opposed to anterior QS waves). Look at R-wave amplitude, T-wave size and morphology (especially hyperacute, upright T-waves for acute STEMI), and degree of ST Elevation (which should only be moderate in aneurysm morphology). Perform an echo, obtain serial ECGs, and always if possible compare to a prior ECG.
2. If despite taking these measures, the diagnosis is still in doubt: err on the side of cath lab activation!
3. Beware of ACS presenting with atypical symptoms, including absence of chest pain. This is particularly true in women, diabetics, and the elderly. You can see from this case that one can have Massive MI and still not experience any chest pain!