Preface
This was sent by a medical student somewhere in the world who will remain anonymous. Details are scant so that it cannot be recognized.
The minute this medical student saw the first ECG, he knew the diagnosis without any further information. Reading ECGs is hard, but can be done with commitment to learning, which comes from an awareness of its importance. My most talented blog readers are paramedics because they have to put themselves on the line every time they activate the cath lab. And they teach me a lot.
One of my most talented readers is a health care assistant (a nursing assistant) who has taken a keen interest in ECGs. He can beat nearly anyone. So you don't have to be highly trained. You don't have to be a genius. You need to be interested and understand the value of the ECG.
It is not the ECG which is nonspecific, it is the interpreter.
Case
A female in her 60s presented with 3 days of nausea, vomiting, and diarrhea, and not feeling well. She complained of jaw pain and shortness of breath. There was a 30 second episode of syncope, and another one the previous evening, without any tonic clonic movements, tongue-biting, or incontinence. She was ill appearing. She had a remote history of lung cancer many years ago, cured. She had no other medical history.
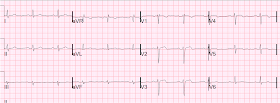
She had this ECG recorded:
 |
| ECG 1: QTc is 484. What do you think, especially compared to the previous, pasted below? |
 |
| Previous ECG. completely normal |
The diagnostic features of the first ECG were entirely missed by a whole team of emergency physicians, cardiologist, surgeons and others, even as the patient became increasingly hypotensive to a systolic BP of 60. The lactate was elevated and pH low. They were worried that the syncope was seizure and that she had brain mets. Then they were worried about sepsis as an etiology of hypotension. Then the notes mention "cardiogenic shock" but without any reference to a cardiac echo or to a chest x-ray. Was there pulmonary edema? Not mentioned in physicians' notes. Then she had some RUQ tenderness which led to a long process of evaluation for an abdominal source of sepsis, which turned up negative. Initially fluids were given, then stopped in favor of pressors, as a CVP line showed CVP = elevated.
Another ECG was recorded:
 |
| ECG 2: Findings are still present and have evolved to a small degree |
At time 6 hours, Troponin T returns at between 0.50 and 1.00 ng/mL (not giving exact number, but significantly high)
Now having frequent PVCs.
Now chest pain free. Cardiologist note says: "Elevated troponin explained by type II MI due to her shock." "Repeat ECG showing no STEMI, only non-specific ST-segment and T-wave abnormalities, unchanged from prior"
Transferred to surgery for exploration but diagnostic studies were too indeterminate to be certain of intra-abdominal pathology. Besides, the surgeons say she is "too unstable for surgery."
Day 2:
A cardiac echo was done which showed normal LV function but
moderate RV systolic dysfunction and
diastolic septal flattening consistent with
right ventricular volume overload.
Right ventricle: moderately enlarged, hypocontractile free wall, moderate global decrease function.
Trop T now very high, well into the range one sees with a STEMI; very unusual in type II MI.
Still the pieces were not put together.
Another ECG is recorded:
 |
| ECG 3: More evolution, but not recognized. |
I have only shown you 3 of the many ECGs recorded over the 3 days, all of which were diagnostic but not diagnosed.
After midnight (now day 3), she complains of shoulder pain and dyspnea. Troponin was repeated and returned higher still.
She was taken to the cath lab.
What was the diagnosis? See below.
Outcome and Analysis:
ECG 1 is diagnostic of inferior and right ventricular MI. There is a junctional bradycardia. There is less than 1 mm of STE in inferior leads with diagnostic reciprocal ST depression in aVL. Additionally, there is ST elevation in V1 which, in the presence of inferior MI is diagnostic of Right ventricular MI. This is the etiology of the syncope and hypotension and shock and elevated CVP. and right ventricular echo findings.. Furthermore, there are T-wave changes in V2 and V3 which are highly suggestive of ischemia, but difficult to localize: anterior? posterior? right ventricular? In any case, these further support the diagnosis of coronary occlusion or near occlusion. ECG 2 is similar, also with a junctional rhythm that is resulting in inverted P-waves in inferior leads (retrograde). ECG 3 is yet more evolved.
When they finally did it, the cath showed a 100% RCA thrombotic occlusion at the ostium (proximal, before the RV marginal branch), confirming all clinical and ECG findings (except for diarrhea). There was also disease of the LAD and Left circ.
She turned out to not have any abdominal pathology.
All cultures were negative.
There were multiple complications.
This was an inferior and right ventricular MI and once the first ECG was recorded, the diagnosis could have been made: everything about the presentation, after the ECG, screamed this diagnosis.
Comment:
I cannot read the minds of the physicians involved, but I suspect there were two components to the delayed diagnosis:
1. Atypical presentation (nausea, vomting, and diarrhea)
2. Failure to regognize subtle but diagnostic features of the ECG.
Many say generally that the ECG is often a "non-diagnostic" test, or a nonspecific test. Most often, it is the interpreter who is nondiagnostic and nonspecific. The ECG here told the whole story, very specifically. It was the failure of accurate interpretation which led to a 2 day delay in diagnosis and significicant myocardial loss and much unnecessary diagnostic and therapeutic intervention.
The ECG told the whole story, but no one listened.