Case 1
Below are 2 cases of circumflex or obtuse marginal (branch of circumflex) occlusions showing how subtle they may be:
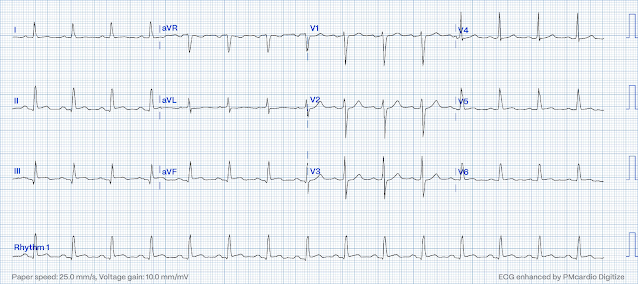
A 52 y.o. male presents because he "thought he might be having a heart attack." He reports intermittent CP and SOB for 2-3 days. Pain worsened and became sharper after lifting a bookcase up the stairs. He continued to have worsening pain and diaphoresis, and associated left arm pain down to the fingers. Pt. reports MI in 2001 with a stent placed in the "marginal" artery. Pain is similar, but associated with less SOB. Exam is unremarkable. Here is the EKG at 1810:
Below are 2 cases of circumflex or obtuse marginal (branch of circumflex) occlusions showing how subtle they may be:
A 52 y.o. male presents because he "thought he might be having a heart attack." He reports intermittent CP and SOB for 2-3 days. Pain worsened and became sharper after lifting a bookcase up the stairs. He continued to have worsening pain and diaphoresis, and associated left arm pain down to the fingers. Pt. reports MI in 2001 with a stent placed in the "marginal" artery. Pain is similar, but associated with less SOB. Exam is unremarkable. Here is the EKG at 1810:
A repeat ECG 1 hour later is subtly changed, with some evolving T-wave inversion best seen in V5 and V6.
This is diagnostic of inferior and lateral OMI, possibly with reperfusion since the T-waves are inverted.Here is the PM Cardio Digitization:
I sent this ECG to the Queen of Hearts (PMcardio OMI), and here is the verdict:
OMI with High Confidence
A stat echocardiogram would have helped to make this diagnosis and facilitate timely reperfusion. Angiography and PCI were undertake 8 hours after the initial ECG and showed a completely occluded OM-1. Echo revealed inferior-posterior wall motion abnormality and 4th generation troponin I peaked at over 100 ng/mL (A huge OMI)!
It is not unusual for occlusions of the circumflex or its branches to show little on the ECG even though they represent a large amount of ischemic myocardium at risk for complete infarction. The circumflex territory is known as being "electrocardiographically silent".
How can you make the diagnosis? First, this patient had a known stent in the "marginal" artery and thought he was having a heart attack. In such a situation, when you know that the circumflex is the likely culprit artery, you may suspect that an MI will not be obvious on the ECG. In this case the ECG was diagnostic of OMI. But if you don't see it and don't have the Queen of Hearts, additional diagnostic testing is warranted. Possibilities include: serial ECGs (which were done but still nondiagnostic), stat echocardiogram, or posterior ECG. Use of the PRIME ECG 80 lead body surface mapping shows great potential for improving diagnosis in such cases.
By definition, this is a non-STEMI because there is not 1 mm of ST elevation in 2 consecutive leads. However, ST elevation is only an imperfect surrogate for complete acute persistent occlusion of an epicardial coronary artery without collateral circulation. It is neither fully sensitive nor specific. Even though the patient's ECG did not meet criteria for STEMI, this OMI had all the pathology of a STEMI.
Case 2
A 38 year old male with h/o smoking only c/o a few hours of severe substernal chest pain; he thinks he is having a heart attack. The pain is very nitroglycerine responsive. The first ECG with pain (unavailable) showed T wave flattening in V2 and V3. After resolution of pain with sublingual nitroglycerine, the second ECG was changed to near normal:
I sent this ECG to the Queen of Hearts (PMcardio OMI), and here is the verdict:
73 minutes later, the patient developed pain again:
Not OMI with High Confidence
73 minutes later, the patient developed pain again:
This again is highly suggestive of inferior OMI.
I sent this ECG to the Queen of Hearts (PMcardio OMI), and here is the verdict:
Not OMI with Low Confidence
Nitroglycerine again eventually resolved the pain, and the following ECG was recorded at 2234:
There is reperfusion in inferior leads and a large T-wave in V2 (posterior reperfusion)
This change makes it clear that the findings on the 2nd ECG were indeed due to OMI!!
These T-waves represent reperfusion of the posterior wall, what I call "posterior reperfusion T-waves." Click here for more such cases.
The troponin I returned at 0.81 ng/ml, so the patient was started on heparin and eptifibatide, in addition to IV nitroglycerine and Metoprolol (and, of course, aspirin).
His angiogram the next day revealed a 100% mid dominant circumflex occlusion that supplied the inferior and posterior walls. There was a large LAD that collaterally supplied some of the inferior wall. Echo showed an inferior-posterior wall motion abnormality. The troponin peaked at only 13 ng/mL, probably because of the collateral circulation from the LAD.
How could we have gotten him to angiography and PCI faster? Patients with objective evidence of acute coronary syndrome (positive troponin or ECG) AND uncontrollable pain should get emergent PCI even if they do not have ST elevation. This patient did become pain free on maximal medical therapy, so PCI was not indicated.
Fortunately, his MI was not huge by biomarkers, but it was large (most OMI are higher than 10 ng/mL of Troponin I). Although he had a wall motion abnormality, this may go away over time.

.jpeg)
.jpeg)
.jpeg)
.jpeg)
.jpeg)